Certain cancers are more painful than most.
And most types of cancer, especially in the later stages (stage 4), are painful.
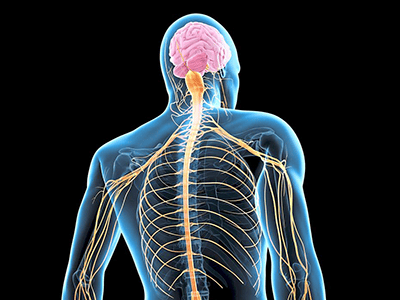
Among the most painful types of cancer are bone cancer, head and neck cancer, and brain and spinal cord cancer.
The presence of pain depends mainly on the location of the cancer and the stage of the disease.
Pain in cancer may arise from a tumour compressing or infiltrating nearby body parts; treatments and diagnostic procedures; or changes to skin, nerves and other tissues caused by a hormone imbalance or immune response.
However, the pain from most types of cancer can be controlled.
While most cancer pain can be managed with pharmacological treatment (using drugs such as opioids, anti-neuropathics, anti-depressants, etc), about 10% to 20% of cancer pain would need other methods, such as interventional pain management techniques and other non-pharmacological techniques like psychosocial management, physiotherapy techniques, and traditional and complementary medicine.
Pain management is important in palliative care.
Palliative therapy represents active care for patients whose illness is not responding to the curative treatment.
It aims to provide comfort and prevent the suffering of patients, especially towards the end of their life.
Thus, treatment of the pain presents an important integral part of palliative care.
Proper pain management can achieve a better quality of life for patients and their families.
Meanwhile, poor pain management has been shown to increase complications and reduce a patient’s life expectancy.
Proper assessment required
Patients with cancer pain need to undergo a comprehensive assessment of their pain.
This is the first step to achieving successful cancer pain management.
Similar to other clinical assessments, a complete pain assessment requires a detailed medical history, physical examination and relevant investigations.
The assessment aims to determine the nature and pathophysiology of the pain, severity of the pain, impact of the pain on functions and quality of life, and the response to interventions.
From the assessment, a plan can be formulated to help treat the patient’s pain.
Methods of pain management
Managing cancer pain is highly complex. It can be divided into pharmacological treatment, anti- cancer treatments, non-pharmacological methods and interventional techniques.
Pharmacological treatment includes using drugs such as opioids (e.g. morphine), drugs to treat neuropathic pain (anti-epileptics, antidepressants etc), and steroids.
Non-pharmacological methods include exercise therapy, psychosocial therapy, and traditional and complementary medicine (e.g. acupuncture).
Anti-cancer treatment includes radiotherapy and chemotherapy.
Meanwhile, there is a wide range of interventional techniques available for the relief of cancer pain.
These methods should be considered when conventional therapy, as mentioned above, fails to provide adequate pain control.
Examples of interventional techniques are nerve blocks, neurolysis, and insertion of an intrathecal morphine pump.
A nerve block is done by injecting local anaesthetics – sometimes combined with steroids – to block sensation to an area of the body.
For instance, if a patient has bone cancer of the arm, we would inject local anaesthetics around the nerve that supplies the arm in order to stop the pain sensation there.
However, the application of local anaesthetics may not last long due to the drugs’ limited time effect, thus, this is usually done for diagnostic purposes.
Neurolysis is a technique that is used to alleviate pain.
It is done either by using chemical agents (e.g. alcohol or phenol) or thermal techniques (e.g. radiofrequency ablation) on the nervous system.
Neurolysis is only used when the disease has progressed to a point where no other pain treatments are effective.
And an intrathecal pump is a device that delivers small quantities of pain medication such as morphine, directly to the spinal fluid.
When these drugs are used and delivered in smaller doses, it may minimise the side effects often experienced with larger oral doses of the same medications, and patients may also experience better pain relief.
Patients who should be considered for these interventions include those with significant pain from locally- advanced disease, severe neuropathic pain, and severe pain on movement.
Challenges in pain management
There are barriers to effective pain management in cancer patients, including:
- Restrictive policies governing healthcare practice.
- Regulatory scrutiny when prescribing controlled substances.
- Lack of knowledge among patients, healthcare providers and caregivers about cancer pain management.
- The use of religious and cultural strategies to cope with pain.
- Inadequate attention to pain in certain patient populations, and
- Patient concerns about addiction and the harmful effects of pain treatment.
Although effective cancer pain management is highly recommended, the patient’s cultural beliefs may ingrain a deep pain tolerance, thus discouraging effective treatment of cancer pain.
Some cultural and religious beliefs may discourage the use of certain pain management methods, such as medications, while others uphold alternative therapies or spiritual practices to cope with pain.
Some examples would be:
Belief in karma
In many cultures, pain and suffering are perceived as a result of past actions and may be necessary for spiritual growth.
This belief can result in patients not seeking treatment or not reporting their pain because they feel that it is deserved.
Belief in spiritual healing
Spiritual practices such as prayer or meditation, are believed to be more effective at managing pain than medications.
While these practices can provide some relief, they may not be sufficient for more severe or chronic pain.
Some also believe that certain medications or medical procedures are “impure” or interfere with spiritual purity.
Fear of addiction
Some cultures and religions view pain medications as addictive, and therefore, discourage its use.
This can result in patients not receiving adequate pain relief because they are afraid of becoming addicted to such medications.
Relieving the suffering
Expertise in pain management techniques is continuously growing.
Hence, healthcare professionals should be aware of their roles and appropriately refer their patients to specialists who are trained in pain management where available.
To a cancer patient, the pain he or she feels can stand in the way of positive treatment outcomes.
When the pain is managed and becomes bearable – if not gone altogether – the patient’s focus can shift from one of suffering to one of hopefulness.
This article first appeared in The Star, 10 May 2023.
Share:
Was this article helpful?
Share:
Was this article helpful?
Health Packages
Elevate your health with tailored health packages at Columbia Asia Hospital. Take charge of your health journey today.