15 October 2018
•5 minute read
The Many Ways Diabetes Affects Your Eyes
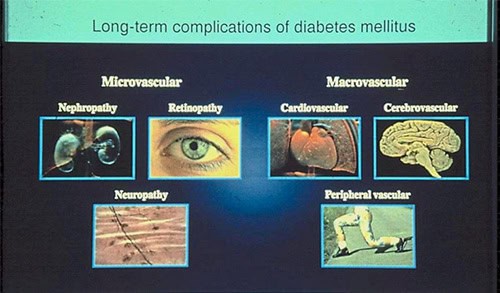
Diabetes can affect the eyes in many ways. Diabetic retinopathy affects blood vessels in the light-sensitive tissue called the retina that lines the back of the eye.
It is the most common cause of vision loss among people with diabetes and the leading cause of vision impairment and blindness in adults.
This condition usually develops in anyone who has poorly controlled type 1 or type 2 diabetes.
Diabetic eye diseases also include cataract and glaucoma:
- Cataract: Adults with diabetes are two to five times more likely than those without diabetes to develop cataract. It also tends to develop at an earlier age.
- Glaucoma: Certain types of glaucoma are associated with elevated pressure inside the eye. In adults, diabetes nearly doubles the risk of glaucoma.
All forms of diabetic eye disease have the potential to cause severe vision loss and blindness.
Types of diabetic retinopathy
There are three types of diabetic retinopathy:
- Non-proliferative retinopathy is an early form of the disease, where the retinal blood vessels leak fluid or bleed.
- Macular oedema is a swelling of the macula, caused by the leakage of fluid from retinal blood vessels. It can damage central vision.
- Proliferative retinopathy is an advanced form of the disease and occurs when blood vessels in the retina disappear and are replaced by new fragile vessels that bleed easily. This can result in a sudden loss of vision.
One might not have symptoms in the early stages of diabetic retinopathy. It usually affects both eyes.
As the condition progresses, symptoms may include:
- Spots or dark strings floating in your vision (floaters).
- Blurred vision.
- Fluctuating vision.
- Impaired colour vision.
- Dark or empty areas in your vision.
- Vision loss.
What causes diabetic retinopathy?
Chronically high blood sugar from diabetes is associated with damage to the tiny blood vessels in the retina, leading to diabetic retinopathy.
It can cause blood vessels in the retina to leak fluid or haemorrhage (bleed), distorting vision.
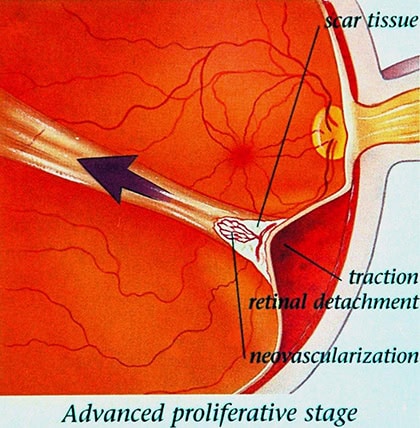
In its most advanced stage, new abnormal blood vessels proliferate (increase in number) on the surface of the retina, which can lead to scarring and cell loss in the retina.
Diabetic retinopathy may progress through four stages:
- Mild non-proliferative retinopathy
- Moderate non-proliferative retinopathy
- Severe non-proliferative retinopathy
- Proliferative diabetic retinopathy (PDR).
At this advanced stage, growth factors secreted by the retina trigger the proliferation of new blood vessels, which grow along the inside surface of the retina and into the vitreous gel, the fluid that fills the eye.
The new blood vessels are fragile, which makes them more likely to leak and bleed.
Accompanying scar tissue can contract and cause retinal detachment – the pulling away of the retina from underlying tissue, like wallpaper peeling away from a wall. This can lead to permanent vision loss.
The risk of developing diabetic retinopathy can increase as a result of:
- Duration of diabetes – The longer one has diabetes, the greater risk of developing diabetic retinopathy.
- Poor control of blood sugar level.
- High blood pressure.
- High cholesterol levels.
- Pregnancy.
- Smoking.
Diabetic retinopathy and diabetic macular oedema are detected during a comprehensive dilated eye exam that includes:
- Visual acuity testing.
- Pupil dilation – allowing a physician to examine the retina and optic nerve.
- Optical coherence tomography (OCT) – Scanning of the nerve fibre layers.
A comprehensive dilated eye exam allows the doctor to check the retina for:
- Changes to blood vessels.
- Leaking blood vessels or warning signs of leaky blood vessels, such as fatty deposits.
- Swelling of the macula (DME).
- Changes in the lens.
- Damage to nerve tissue.
Complications of diabetic retinopathy
Complications can lead to serious vision problems such as:
- Vitreous haemorrhage – The new blood vessels may bleed into the clear, jelly-like substance that fills the centre of eye.
If the amount of bleeding is small, one might see only a few dark spots (floaters).
In more severe cases, blood can fill the vitreous cavity and completely block vision.
- Retinal detachment – The abnormal blood vessels associated with diabetic retinopathy stimulate the growth of scar tissue, which can pull the retina away from the back of the eye, which will cause severe vision loss.
- Glaucoma – New blood vessels may grow in the front part of your eye and interfere with the normal flow of fluid out of the eye, causing pressure in the eye to build up.
- Blindness – Eventually, diabetic retinopathy, glaucoma or both can lead to complete vision loss.
RISIKO KEPADA BAYI
Preventing diabetic retinopathy
Regular eye exams, good control of your blood sugar and blood pressure, and early intervention for vision problems can help prevent severe vision loss.
- Manage your diabetes. Make healthy eating and physical activity a part of your daily routine.
- Take oral diabetes medications or insulin as directed.
- Monitor blood sugar level. You may need to check and record your blood sugar level several times a day.
- Keep blood pressure and cholesterol under control.
- Stop smoking. Smoking increases the risk of various diabetes complications, including diabetic retinopathy.
- Pay attention to vision changes.
Treating diabetic retinopathy
Vision lost to diabetic retinopathy is sometimes irreversible. However, early detection and treatment can reduce the risk of blindness by 95%.
Because diabetic retinopathy often lacks early symptoms, people with diabetes should get a comprehensive dilated eye exam at least once a year.
People with diabetic retinopathy may need eye exams more frequently, and women with diabetes who become pregnant should have a comprehensive dilated eye exam as soon as possible.
Additional exams during pregnancy may be needed.
Early diabetic retinopathy – If one has mild or moderate non-proliferative diabetic retinopathy, one may not need treatment right away.
However, the eye doctor will closely monitor the eyes to determine when you might need treatment.
Work with a diabetes doctor (endocrinologist) to determine if there are ways to improve diabetes management. When diabetic retinopathy is mild or moderate, good blood sugar control can usually slow the progression.
Advanced diabetic retinopathy – If one has proliferative diabetic retinopathy or macular oedema, one will need prompt surgical treatment.
Photocoagulation, also known as focal or grid laser treatment, can stop or slow the leakage of blood and fluid in the eye.
During the procedure, leaks from abnormal blood vessels are treated with laser burns. It is usually done in an eye clinic.
Panretinal photocoagulation, also known as scatter laser treatment, can shrink abnormal blood vessels.
During the procedure, the areas of the retina away from the macula are treated with scattered laser burns. The burns cause the abnormal new blood vessels to shrink and scar.
Some loss of peripheral vision or night vision after the procedure is possible.
In vitrectomy, a tiny incision is made in the eye to remove blood from the middle of the eye (vitreous), as well as scar tissue that’s tugging on the retina.
It’s done in a surgery centre or hospital using local or general anaesthesia.
The eye doctor may also suggest injecting medication into the vitreous of the eye.
These medications, called vascular endothelial growth factor (VEGF) inhibitors, may help stop growth of new blood vessels by blocking the effects of growth signals the body sends to generate new blood vessels.
The doctor may recommend these medications, also called anti-VEGF therapy, as a stand-alone treatment or in combination with panretinal photocoagulation.
All the above treatments slow or stop the progression of diabetic retinopathy, but it’s not a cure. Because diabetes is a lifelong condition, future retinal damage and vision loss are still possible.
The Many Ways Diabetes Affects Your Eyes – The Star, 8 October 2018.
Share:
Was this article helpful?
15 October 2018
•5 minute read
The Many Ways Diabetes Affects Your Eyes
Articles and Video
Learn more about Ophthalmology in Columbia Asia
Learn MoreShare:
Was this article helpful?
Health Packages
Elevate your health with tailored health packages at Columbia Asia Hospital. Take charge of your health journey today.